Understanding Alzheimer’s Disease: The Need for Novel Approaches
Alzheimer’s disease is characterized by the accumulation of amyloid-beta plaques and tau protein tangles in the brain, leading to the loss of neurons and cognitive decline. Conventional drug therapies primarily target these pathological hallmarks, but their success in halting disease progression remains limited. Additionally, some medications come with adverse side effects, leaving patients and their caregivers in search of safer and more effective alternatives.
Enter Brain Photobiomodulation: Shedding Light on Hope
Brain photobiomodulation, also known as transcranial photobiomodulation (tPBM) or low-level light therapy, involves applying specific wavelengths of light to the scalp to stimulate cellular function within the brain. This non-invasive technique has gained traction as a potential therapeutic tool for various neurological conditions, including Alzheimer’s disease.
How Brain Photobiomodulation Works
During brain photobiomodulation, near-infrared light is delivered to targeted areas of the brain. This light penetrates the skull and is absorbed by mitochondria within neurons and other cells. Mitochondria, often referred to as the “powerhouses” of cells, produce adenosine triphosphate (ATP), which is essential for cellular energy and function. By enhancing mitochondrial activity, brain photobiomodulation promotes cellular health and can have beneficial effects on neuronal function and communication.
Promising Research and Results
Preliminary studies investigating the effects of brain photobiomodulation on Alzheimer’s disease have shown encouraging outcomes. Researchers have observed improvements in cognitive performance, memory, and learning abilities in animal models with Alzheimer’s-like pathology. Human clinical trials are ongoing and have reported positive trends, suggesting that brain photobiomodulation may slow cognitive decline and improve certain aspects of memory in individuals with mild cognitive impairment or early-stage Alzheimer’s disease.
Potential Mechanisms of Action
The exact mechanisms by which brain photobiomodulation exerts its therapeutic effects on Alzheimer’s disease are still being explored. Some proposed mechanisms include:
- Reduction of Neuroinflammation: Brain photobiomodulation may help reduce inflammation in the brain, which is known to play a significant role in the progression of Alzheimer’s disease.
- Enhancement of Blood Flow: By improving blood flow and vascular function, brain photobiomodulation may support the delivery of nutrients and oxygen to brain cells, aiding their survival and function.
- Stimulation of Brain Plasticity: Brain photobiomodulation might enhance neuroplasticity, the brain’s ability to reorganize and form new connections, which could lead to cognitive improvements.
Safety and Accessibility
One of the major advantages of brain photobiomodulation is its non-invasiveness and lack of reported serious side effects. It offers a drug-free approach that is relatively safe and well-tolerated, making it an attractive option for individuals seeking alternatives to traditional medications.
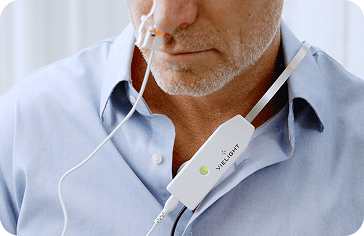
Moreover, the equipment required for brain photobiomodulation is becoming increasingly accessible, with portable devices available for home use. However, it is crucial to consult with healthcare professionals before using such devices to ensure proper usage and safety.
The Way Forward: Expanding Research and Awareness
While brain photobiomodulation shows great promise as a drug-free alternative for treating Alzheimer’s disease, it is essential to recognize that research in this area is still in its early stages. More comprehensive clinical trials and long-term studies are needed to establish the therapy’s efficacy and safety conclusively.
Published Brain Photobiomodulation Research for Alzheimer’s and Dementia with Vielight technology
In 2015, our dementia pilot trial made history by being the first to show efficacy of brain photobiomodulation (PBM) for dementia in humans with a home-use device.[1]
In 2019, Dr. Linda Chao, a professor in the Departments of Radiology, Biomedical Imaging and Psychiatry at the University of California, verified our 2015 dementia pilot trial with her own independent brain photobiomodulation study with the Vielight Neuro Gamma on participants with dementia.[2]
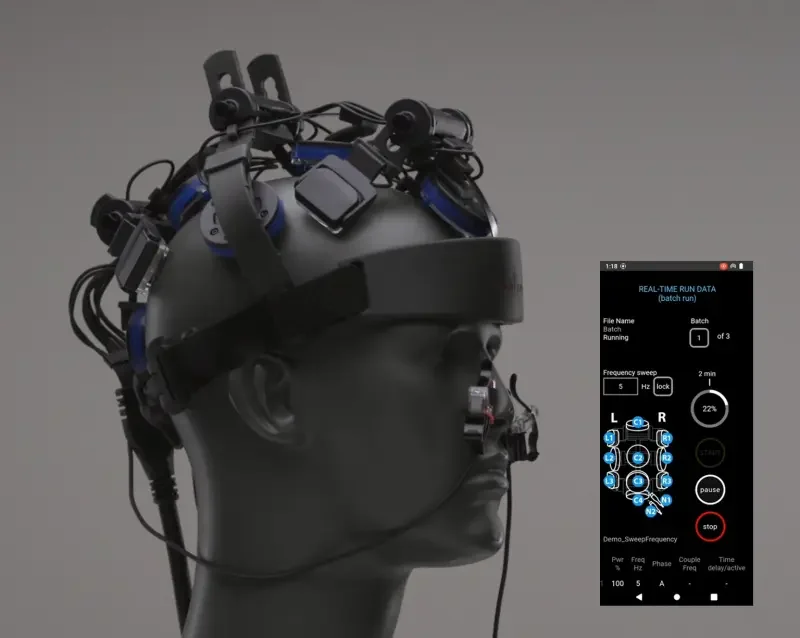
Eight participants diagnosed with dementia were randomized to 12 weeks of usual care or home photobiomodulation(PBM) treatments. The PBM treatments were administered at home with the Vielight Neuro Gamma, a brain photobiomodulation device that emits 100 mW/cm2 of power density at 810nm and 40hz.